To reliably determine the Epstein Barr virus, it is necessary to detect antibodies to it in the patient's blood. So you can accurately start the treatment of pathology.
Contact of the human body with any infection causes an immune response. Lymphocytes produce specific proteins that attach to a virus or bacteria and present them to cells, which destroy foreign organisms. Some proteins remain on the cell membranes of lymphocytes and form a kind of memory for the immune system. After infection with herpes type 4, antibodies to the Epstein-Barr virus are produced.
Infection occurs through household or airborne droplets. It is implemented by the following mechanisms:
Primary infection in most cases is asymptomatic or with mild catarrhal symptoms. Only 20% manifest as primary infectious mononucleosis. Later, in 15% of those infected, the infection proceeds chronically with relapses.
At different periods of the disease, antibodies to the Epstein virus are synthesized - these are proteins of the immunoglobulin class, which, depending on the type and concentration in the blood, indicate an acute or past infection.
EBV leads to the following diseases:
- Infectious mononucleosis;
- herpes;
- multiple sclerosis;
- tumors of the salivary glands;
- lymphoorganulomatosis;
- lymphoma.
Pathogenesis
The virus enters the mucous membrane of the nasopharynx and respiratory tract, multiplies in the epithelium and infects neighboring cells and lymphocytes. In some of the affected B-lymphocytes, the Epstein virus divides, while in the rest it remains dormant. At the initial stages, T and NK cells are also infected, a chronic infection occurs with the circulation of the virus in lymphocytes.
This is how the mechanism of avoiding the immune response is realized. It produces proteins that are identical in amino acid sequence to interleukin-10, which leads to inhibition of the synthesis of interferon-gamma.
These mechanisms help to avoid the reaction of the immune system when the infection is activated, cause immunodeficiency and manifestation of the secondary flora.
Diagnostics
Three types of antibodies form the basis of the immune response:
- capsid, or VCA;
- nuclear EBNA to the nuclear antigen of the virus;
- early EA.
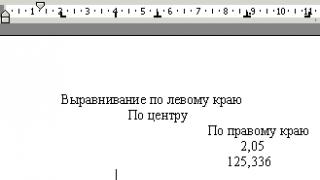
Antibodies to the Epstein-Barr virus belong to the IgM and IgG types. According to the staging of the appearance of AT to determine the period of infection - primary, transferred or reactivated. 
For the study, blood serum (ELISA), biological fluids - saliva, bone marrow, blood (PCR) are used. Antibodies can be detected using enzyme immunoassay, and virus DNA can be detected through PCR.
Early EA belongs to the IgG class, the maximum concentration falls on the 2nd week of illness, then it completely disappears within 3-5 months.
After infection in 100% of cases will find IgM against the capsid of the virus. They increase from the first week, reach a maximum by 3, then gradually decrease. They are determined in serum up to 6 months after contact with the pathogen. A positive IgM VCA class indicates an exacerbation of the disease.
Antibodies to the Epstein-Barr virus IgG VCA appear early, already at 1-4 weeks, and increase to the maximum by 2 months of illness. After recovery, their titer gradually decreases, but can be recorded for several more years after recovery. VCA IgG speak about the state after the disease and the formation of immunity.
Acute primary infection reflects elevated concentrations or a gradual increase in VCA IgG.
Antibodies to the nuclear antigen appear at 4 weeks after infection and never in the early phase. Their appearance reflects the stage when the Epstein virus has invaded the cell nucleus. They increase, gradually stabilize at the 3rd month of infection. In the future, they are determined throughout life.
The combination of antibodies is treated as follows.

Virus rate
Deciphering the result is necessary for the doctor to correlate these analyzes with clinical manifestations and make a diagnosis. Immunoglobulin is quantified. The following indicators are significant:
- negative - less than 20 U / ml;
- doubtful - 20-40 U / ml;
- positive - more than 40 U / ml.
A positive analysis can be in the following cases:
- acute infection in the last 1-2 months;
- reactivation of the virus;
- chronic infection with constant activity.
A negative study response can be interpreted as follows:
- no infection;
- incubation period;
- early or late persistent infection;
- atypical infection or reactivation of the process.
In some cases, it may be difficult to diagnose and interpret the results. Class M antibodies to the viral capsid do not always appear before IgG. This is seen with immunosuppression.
Occasionally, IgM persist for a long time in the blood. As a result, in a patient with a paste infection, serological analysis mimics a late primary infection.
Nuclear antigen during deep immune suppression does not provoke the appearance of IgG.
IgG to EA does not always indicate an early period of primary infection. It can be determined in 70% of those with acute mononucleosis and can be detected in healthy people, as well as when the infection is reactivated.
Diseases of the immune system can lead to serious distortions of serological analysis. Helps in the diagnosis of determining the DNA of the virus by PCR in biological fluids. The most informative method for the analysis of swabs from the nasopharynx obtained during the first 4 weeks of illness.
High titers of G antibodies to the nuclear antigen, capsid, and early type are often detected in malignant neoplasms associated with EBV infection activity.
Epstein-Barr virus (capsid antigen, VCA), IgG antibodies
Epstein-Barr virus
Lymphocryptovirus subfamilies Gammaherpesvirinae families herpesviridae, has 4 main antigens: early antigen(early antigen - EA), capsid antigen membrane antigen n (membrane antigen - MA); nuclear antigen
Epidemiology
Pathogenesis.
Clinical manifestations. Infectious mononucleosis
1. Recovery.
At immunocompetent patients
Serological diagnosis
|
Indicator |
Characteristic |
|
Material |
Deoxygenated blood |
|
Patient preparation rules |
Standard, see section no. 15 |
|
Transport medium, tube |
|
|
Standard, see section no. 17 |
|
|
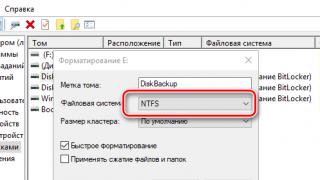
Test method |
Flow cytometry |
|
Analyzer and test system |
BioPlex 2200; BioRad (USA) |
|
Reference values |
|
|
Indications for appointment |
|
|
Interpretation of results |
|
|
Positive result |
Negative result |
|
|
Description:
Epstein-Barr virus
Etiology. Human herpes virus type 4(HHV-IV), or Epstein-Barr virus, is a lymphotropic virus, its etiological role is known in infectious mononucleosis, Burkitt's lymphoma, nasopharyngeal carcinoma, X-linked lymphoproliferative syndrome, and chronic fatigue syndrome. It is a DNA genomic virus of the genus Lymphocryptovirus subfamilies Gammaherpesvirinae families herpesviridae, has 4 main antigens: early antigen(early antigen - EA), capsid antigen(viral capcide antigen - VCA), membrane antigen n (membrane antigen - MA); nuclear antigen(Epstain-Barr Nuclea antigen - EBNA). Each of them is formed in a certain sequence and induces the synthesis of the corresponding antibodies.
Epidemiology. The source of infection is an infected person (with a manifest or erased form of the disease, as well as a virus carrier). Primary infection often occurs in childhood or young age. Ways of transmission of the virus: airborne, contact-household, transfusion, sexual, transplacental. After infection, the replication of the virus in the human body and the formation of an immune response may be asymptomatic or manifest as minor signs of SARS. In some cases, more often if there is a significant weakening of the immune system during this period, the patient may develop a picture of infectious mononucleosis. About 90% of the adult population of the world are infected with the Epstein-Barr virus and after a primary infection remain carriers of the virus for life.
Pathogenesis. The entrance gate for infectious mononucleosis is the mucous membrane of the oral cavity and upper respiratory tract. Epstein-Barr virus penetrates intact epithelial layers by transcytosis into the underlying lymphoid tissue of the tonsils, in particular B-lymphocytes. After infection, the number of affected cells increases through virus-dependent cell proliferation. Infected B-lymphocytes can reside in tonsillar crypts for a significant time, which allows the virus to be released into the external environment with saliva. With infected cells, the virus spreads to other lymphoid tissues and peripheral blood. In virus-infected cells, two types of reproduction are possible: lytic, that is, leading to death, lysis of the host cell, and latent, when the number of viral copies is small and the cell is not destroyed. In acute or active infection, lytic viral replication predominates. The virus can stay in B-lymphocytes and epithelial cells of the nasopharyngeal region and salivary glands for a long time. In addition, it is able to infect other cells: T-lymphocytes, NK cells, macrophages, neutrophils, vascular epithelial cells. In the nucleus of the host cell, the DNA of the virus can integrate into the genome, causing chromosomal abnormalities. Active reproduction of the virus can occur as a result of a weakening of immunological control, as well as stimulation of the reproduction of cells infected with the virus under the influence of a number of factors: acute bacterial or viral infection, vaccination, stress, etc.
Clinical manifestations. Infectious mononucleosis- an acute anthroponotic viral infectious disease characterized by fever, damage to the oropharynx, lymph nodes, liver and spleen, and specific changes in the hemogram. The incubation period of the disease is 4-6 weeks. In the prodromal period, the infection is manifested by muscle pain, fatigue, and general malaise. Then they are joined by fever, sore throat, swollen lymph nodes, spleen and sometimes liver. In some cases, a rash appears on the arms and torso. Symptoms persist for 2-4 weeks. In children, the infection is often asymptomatic. There are several options for the outcome of an acute infectious process:
1. Recovery.
2. Asymptomatic carrier or latent infection.
3. Chronic recurrent infection:
a) chronic active infection (preservation of symptoms of infectious mononucleosis for more than 6 months);
b) generalized form (perhaps damage to the nervous system (encephalitis, polyneuropathy, meningitis), other internal organs (myocarditis, glomerulonephritis, lymphocytic interstitial pneumonia, hepatitis);
c) hemophagocytic syndrome associated with EBV infection;
d) erased or atypical forms (prolonged subfebrile condition of unknown origin, clinic of secondary immunodeficiency - recurrent bacterial, fungal, often - mixed infections of the respiratory and gastrointestinal tract, furunculosis, etc.);
e) the development of an oncological (lymphoproliferative) process (multiple polyclonal lymphomas, nasopharyngeal carcinoma, leukoplakia of the tongue and oral mucosa, cancer of the stomach and intestines, etc.);
f) development of autoimmune processes (SLE, rheumatoid arthritis, Sjögren's syndrome, etc.);
g) Epstein-Barr virus may play an important role in the occurrence of chronic fatigue syndrome.
The prognosis for a patient with an acute infection caused by the Epstein-Barr virus depends on the presence and severity of immune dysfunction, genetic predisposition to EBV-associated diseases, as well as on the influence of external factors (stress, infections, surgical interventions, adverse environmental effects), damaging the immune system.
At immunocompetent patients infected B-lymphocytes are under the control of T-lymphocytes, therefore, in most cases, when the infection is reactivated, the course of the disease remains in a subclinical form. In AIDS patients, cloning of undying B-lymphocytes can cause the development of lymphoma.
Laboratory diagnostics is based on the determination of serological markers of infection and the detection of the virus by PCR in various biological fluids.
Hematological changes resembling the picture of infectious mononucleosis can also be observed with cytomegalovirus infection, toxoplasmosis, acute respiratory viral diseases, chickenpox, measles, infectious hepatitis and other diseases. Therefore, it is advisable to conduct a series of tests for differential diagnosis. Specific serological diagnosis of infection is based on the use of a combination of tests that detect the presence of IgG and IgM antibodies to various antigen proteins of the virus, which, in most cases, makes it possible to differentiate the infection and clarify the stage of the pathological process.
Serological diagnosis
Heterophilic antibodies to the Epstein-Barr virus. The detection of heterophile antibodies is one of the criteria for diagnosing infectious mononucleosis. They belong to the class of immunoglobulins M (IgM) and appear within 1-2 weeks from the onset of clinical manifestations of the disease. In 60% of young people, a positive result is observed after 2 weeks and in 90% after 4 weeks from the onset of clinical manifestations, therefore, to diagnose infectious mononucleosis, it is necessary to conduct studies at the 1st week (the result may be negative) and after 1-2 weeks from the onset clinical manifestations. The level of heterophilic antibodies decreases after the end of the acute period of the infectious process, but their titer can be determined within 9 months after the onset of clinical symptoms. Among children with infectious mononucleosis under the age of 2 years, heterophilic antibodies are detected only in 30% of patients, at the age of 2-4 years - 75%, over 4 years - more than 90%. The concentration of heterophilic antibodies does not cross-react and does not correlate with specific antibodies to EBV, and there is no correlation with the severity of the disease. Test results may be positive for other viral diseases. If heterophilic antibodies are not detected in the presence of clinical manifestations corresponding to infectious mononucleosis, it is necessary to conduct a study to determine Epstein-Barr virus-specific antibodies.
Epstein-Barr virus (early antigens, EA), IgG antibodies. The determination of these antibodies is a test for the early diagnosis of acute primary EBV infection. IgG antibodies to the early EBV antigen appear during the acute period of the primary infection and quickly disappear with recovery. Appear during reactivation, absent in the atypical form of the disease. High titers of antibodies to the early antigen are detected in chronic Epstein-Barr virus infection, cancer and autoimmune diseases caused by the virus, and immunodeficiency states.
Epstein-Barr virus (capsid antigen, VCA), IgM antibodies. Primary EBV infection is defined serologically by the early appearance of IgM VCA antibodies, which may appear before clinical symptoms. High titers occur at 1-6 weeks from the onset of infection, usually disappear after 1-6 months. This type of antibody is also found during reactivation of the infection. The presence of VCA IgM in the absence of anti-EBNA IgG confirms primary infection. Long-term persistence of high titers of these antibodies is characteristic of chronic Epstein-Barr virus infection, tumors caused by chronic Epstein-Barr virus infection, and autoimmune diseases, secondary immunodeficiency states. VCA IgM antibodies are sometimes detected in low titer in the absence of a confirmed recent infection (eg, chronic active EBV infection).
Epstein-Barr virus (capsid antigen, VCA), IgG antibodies. VCA IgG can appear very early (at 1-4 weeks), reaching a peak by 2 months of illness. In the beginning of the disease are found in most cases. Only 20% of patients show a 4-fold increase in titer when examined in paired sera. After recovery, VCA IgG persist for life. The presence of VCA IgG indicates past infection and the presence of immunity to the virus. In children under 7 years of age, VCA IgG antibodies may not be detected. The persistent presence of VCA IgG in high titers indicates the chronic phase of the infection. A negative result from this test usually rules out past infection, although it does not always rule out acute infection if done early in the acute phase when VCA IgG levels are still undetectable. The result of a single test alone cannot serve as a basis for making a diagnosis; it should be considered in conjunction with clinical observations and data from other diagnostic procedures.
Epstein-Barr virus (capsid antigen), IgG antibody avidity. The study of the avidity of class G immunoglobulins (IgG) to the Epstein-Barr virus is a survey method that allows you to determine the degree of effectiveness of the specific interaction between antibody and antigen molecules, the rate of formation of the immune complex and the completeness of neutralization of antigens. Early virus-specific IgG antibodies formed during primary infection are characterized by low avidity, which increases over several weeks or months.
Epstein-Barr virus (nuclear antigen, EBNA), IgG antibodies. Antibodies to the nuclear antigen of the Epstein-Barr virus are rarely detected in the acute phase of the disease, appear during the recovery period (3-12 months from the onset of the disease), and can persist for many years after the disease. The absence of EBNA IgG antibodies in the presence of VCA IgM indicates a current infection, their detection after a previously negative reaction indicates an existing infection. If the antibody titer does not change during the study in dynamics (during the acute period and during recovery), an acute infection caused by the Epstein-Barr virus is excluded. When the Epstein-Barr virus infection is reactivated, a repeated increase in the titer of EBNA IgG antibodies occurs. In patients with asymptomatic infection, detection of EBNA IgG together with VCA IgM and IgG antibodies is used in differentiating the early stage of convalescence from the acute phase of infectious mononucleosis.
Molecular diagnosis of EBV infection. None of the serological tests is exceptionally reliable for diagnosing primary EBV infection. The PCR method is a useful addition to the diagnostic panel for this purpose, especially when used as a confirmatory test in combination with immunology. Determination of EBV by PCR method allows to determine the DNA of the virus in various biological materials (buccal, oropharyngeal, urogenital scrapings, blood, urine, saliva, cerebrospinal fluid). The detection of Epstein-Barr virus DNA in the test material indicates the etiological role of the virus in the development of the disease in the presence of an appropriate clinical picture. However, due to the possible long-term persistence of the virus in the body, it is not always possible to assess its role in the development of the disease.
|
Indicator |
Characteristic |
|
Material |
Deoxygenated blood |
|
Patient preparation rules |
Standard, see section no. 15 |
|
Transport medium, tube |
Vacutainer with/without anticoagulant with/without gel phase |
|
Rules and conditions of transportation, sample stability |
Standard, see section no. 17 |
|
Test method |
Flow cytometry |
|
Analyzer and test system |
BioPlex 2200; BioRad (USA) |
|
Reference values |
|
|
Indications for appointment |
|
|
|
|
Interpretation of results |
|
|
Positive result |
Negative result |
|
|
How to prepare for the analysis:
Blood test
To exclude factors that may affect the results of the study, it is necessary to adhere to the following preparation rules:
- blood for research is given only on an empty stomach!
- before donating venous blood, it is desirable to have 15 minutes of rest;
- 12 hours before the study, you should exclude alcohol, smoking, eating, limit physical activity;
- exclude medication. If it is not possible to cancel the medication, the laboratory must be informed;
- children under 5 years old, before donating blood, be sure to drink boiled water (in portions, up to 150-200 ml, for 30 minutes)
Description
Training
Indications
Interpretation of results
Description
Method of determination Chemiluminescent immunoassay.
Material under study Serum
Marker of current or past Epstein-Barr virus infection.
Specific serological diagnosis of Epstein-Barr virus infection and infectious mononucleosis caused by this virus is based on the use of a combination of tests that detect the presence of IgG and IgM antibodies to various antigens, which makes it possible to differentiate the infection and clarify the stage of the pathological process. The study of even a single taken serum for different types of antibodies can give a fairly accurate idea of the current infection or reactivation, the presence of immunity or susceptibility to infection with the Epstein-Barr virus.
VCA IgG appear shortly after VCA IgM and in the acute stage of infection are found in almost all patients. After recovery, VCA IgG persist for life. When the infection is reactivated, the titers of these antibodies increase. A negative result on this test usually rules out past infection, although it does not always rule out acute infection if the blood sample was drawn early in the acute phase when VCA IgG levels are still undetectable. If clinical suspicion persists in such cases, the study should be repeated after 10 to 14 days to detect seroconversion. A positive VCA IgG result indicates exposure to the virus. An additional study of VCA IgM (test) and EBNA IgG (test), as well as EA-IgG (test) allows you to determine the phase of infection (acute stage, recovery, pastinfection, reactivation). The result of a single test alone cannot serve as a basis for making a diagnosis; it should be considered in conjunction with clinical observations and data from other diagnostic procedures.
The test is used in combination with tests at the Independent Laboratory INVITRO - anti-EA IgG, anti-VCA IgM, anti-EBNA IgG (see table).
Literature
- Infectious diseases in children. Ed. D. Murray. M. Practice, 2006. 928 p.
- Gorgievski-Hrisoho, W Hinderer, H Nebel-Schickel, et. al. Serodiagnosis of infectious mononucleosis by using recombinant Epstein-Barr virus antigens and enzyme-linked immunosorbent assay technology. J Clin Microbiol. October 1990; 28(10): 2305 - 2311.
Training
Indications for appointment
- Laboratory confirmation of the diagnosis in case of clinical suspicion of acute infectious mononucleosis.
- Assessment of the stage of the course of infection, laboratory confirmation of the diagnosis in the clinic of chronic active infectious mononucleosis.
- Diagnosis of lymphoproliferative and oncological diseases associated with the Epstein-Barr virus.
Interpretation of results
The interpretation of test results contains information for the attending physician and is not a diagnosis. The information in this section should not be used for self-diagnosis or self-treatment. An accurate diagnosis is made by the doctor, using both the results of this examination¤ and the necessary information from other sources: history, results of other examinations, etc.
Output format: quantitative.
Units of measurement in the Independent laboratory INVITRO: U / ml.
Reference values:
- > 20 U / ml - positive.
Positive result:
- acute Epstein-Barr virus infection;
- infection in the past;
- reactivation.
Negative result:
absence of Epstein-Barr virus infection;
early acute infection (with clinical suspicion, repeat in dynamics after 10-14 days).
Table. Interpretation of serological data.
| stage of infection | VCA IgM | VCA IgG | EA-IgG | EBNA IgG |
| No infection and most of the incubation period (30 - 50 days) | ||||
| Suspicion of early primary infection | - | |||
| Acute primary infection | ||||
| Recent infection (less than 6 months) | ||||
| past infection | ||||
| Chronic infection or its reactivation | ||||
| Malignant neoplasms associated with the Epstein-Barr virus | ++++ |
Questions
and answers
What is the Epstein-Barr virus and what diseases does it cause?
Epstein-Barr virus (EBV) belongs to the family of herpes viruses type 4. EBV infection reaches 90% in the age group over 40 years. The virus is transmitted by airborne, sexual, parenteral and transplacental (from mother to fetus) route.
EBV infects B-lymphocytes, simultaneously activating their reproduction, which causes the development of chronic latent infection. It can cause infectious mononucleosis, Burkitt's lymphoma, nasopharyngeal carcinoma, and chronic fatigue syndrome.
To diagnose EBV infection and determine its stage, a set of tests is used:
Did the answer help you?
Not really
What tests should be done to diagnose infectious mononucleosis?
Infectious mononucleosis is a disease caused by the Epstein-Barr virus (EBV), which belongs to the type 4 herpesvirus family.
The incubation period lasts from 4 to 7 weeks. The acute phase is characterized by high body temperature, swollen lymph nodes, lesions of the oropharynx and nasopharynx, enlargement of the liver and spleen, rash on the face, trunk and extremities. The duration of the acute phase of the disease is usually 3-4 weeks, but may be longer. In addition, the infection can occur with mild symptoms of acute respiratory infections, and in some cases asymptomatic and be detected incidentally in a laboratory study, which includes:
- No. 1515 Clinical blood test;
- No. 186 Antibodies of the IgM class to the EBV capsid antigen (VCA-IgM);
- No. 275 Antibodies of the IgG class to the EBV capsid antigen (VCA IgG);
- No. 187 Antibodies of the IgG class to the nuclear antigen of EBV (EBNA IgG);
- No. 255 Antibodies of the IgG class to the early antigen of EBV (anti-EBV EA-D IgG);
- No. 351KR VEB, determination of DNA in blood.
Did the answer help you?
Not really
In this section, you can find out how much it costs to complete this study in your city, read the description of the test and the table for interpreting the results. When choosing where to take the analysis “Anti-Epstein-Barr viral capsid antigens IgG, EBV VCA IgG)” in Moscow and other cities of Russia, do not forget that the price of the analysis, the cost of the procedure for taking biomaterial , methods and terms of examinations in regional medical offices may differ.
Analysis for the Epstein-Barr virus is an important diagnostic element, especially given the high prevalence of such an infection throughout the world. Statistics claim that up to 90% of the entire population of the Earth were exposed to this pathogen in one form or another, and most people after communicating with this virus become its lifelong carrier and source of infection.
Such a prevalence of infection sometimes misleads a person, and he considers an analysis for the Epstein-Barr virus unnecessary. However, this assertion is incorrect. These tests are simply necessary when planning a pregnancy in order to protect the unborn child, they are needed by everyone who has a suspicion of infection, to identify a number of infectious lesions and prevent undesirable health consequences.
Essence of infection
 Epstein-Barr virus (EBV) is a type of herpesvirus, namely the human herpesvirus type IV. When infected, the pathogen enters the epithelium of the oropharynx and salivary gland, provoking an active infection, which is expressed in the presence of the virus in saliva. Further, it spreads to the epithelium of the nasopharynx and affects B-lymphocytes, without affecting blood T-lymphocytes. When exposed to a virus, lymphocytes are able to mutate with the appearance of clones in the form of atypical lymphocytes. Once in the body, EBV provokes a response of the immune system of both humoral and cellular type.
Epstein-Barr virus (EBV) is a type of herpesvirus, namely the human herpesvirus type IV. When infected, the pathogen enters the epithelium of the oropharynx and salivary gland, provoking an active infection, which is expressed in the presence of the virus in saliva. Further, it spreads to the epithelium of the nasopharynx and affects B-lymphocytes, without affecting blood T-lymphocytes. When exposed to a virus, lymphocytes are able to mutate with the appearance of clones in the form of atypical lymphocytes. Once in the body, EBV provokes a response of the immune system of both humoral and cellular type.
The virus has four main antigens: early (appears in the nucleus and cytoplasm), capsid (present in the nucleocapsid), membrane and nuclear (contains polypeptides) types. 2 characteristic strains, A and B, were identified. During the period of long-term existence of EBV, it can be in a chronic (most common), slowly developing and latent form; the chronic form periodically recurs with an acute phase.

- chronic fatigue syndrome;
- mononucleosis (including adenosis, glandular fever, Filatov's disease);
- Hodgkin's disease;
- Burkitt's lymphoma;
- nasopharyngeal carcinoma;
- Stevens-Johnson syndrome;
- hepatitis;
- herpes;
- herpangina;
- multiple sclerosis;
- leukoplakia;
- Kikuchi disease.
The most common manifestation is in the form of an acute form of infectious mononucleosis.
Principle of analysis
Determination of the content of EBV is usually carried out on the basis of (ELISA). The principle of such a study is based on the fact that for any antigen of a pathogenic pathogen, the immune system produces an immunoglobulin (antibody) to block and neutralize a foreign cell. At the first acquaintance with the infection, an antibody of the M group (lgM) is produced, and to counteract the rooted virus, class G antibodies (lgG) are produced.
A blood or saliva test can detect both types of immunoglobulins, and by their level, assess the presence of an infection in the body. The interpretation of the analysis is based on the fact that a high level of their content is recognized as a positive result (there is an infection in the body), and a negative result is a significantly reduced number of them, which indicates that there is no need to produce antibodies.
Epstein-Barr virus antibodies
 Taking into account the presence of 4 EBV antigens, the formation of corresponding antibodies should be expected, their content is typical for a different lesion by this pathogen. Immunoglobulin lgM to the capsid type antigen (VCA) is actively produced during the acute phase of EBV infection. Its content increases rapidly in the initial period of infection and practically disappears after 30-40 days of illness, but reappears during relapses. IgG antibodies replace lgM and can remain for life, even after complete recovery, and with the next exacerbation or re-infection, their number increases.
Taking into account the presence of 4 EBV antigens, the formation of corresponding antibodies should be expected, their content is typical for a different lesion by this pathogen. Immunoglobulin lgM to the capsid type antigen (VCA) is actively produced during the acute phase of EBV infection. Its content increases rapidly in the initial period of infection and practically disappears after 30-40 days of illness, but reappears during relapses. IgG antibodies replace lgM and can remain for life, even after complete recovery, and with the next exacerbation or re-infection, their number increases.
To other antigens, mainly antibodies of the lgG type are produced. Immunoglobulins to the early type antigen (EA) are produced at the initial stage of the acute phase. They appear within a few days after infection, and disappear after 4-6 months.
IgG antibodies to the nuclear type antigen (EBNA) reach a detectable level 4-5 months after infection, even if the disease is asymptomatic.
Basically, they remain in the body for a very long time, so they can be detected in almost 90% of adults. With the activation of the disease, an increase in the level of lgG EBNA is observed. Their increased background may indicate a chronic form of the development of the disease.
Carrying out analyzes based on ELISA
 Determination of the presence of antibodies is carried out on samples of venous blood and saliva. In the absence of infection, antibodies are not detected. In the acute form of the disease, lgM VCA is found; lgG VCA and lgG EA may be present; lgG EBNA is missing. In the acute phase of the chronic form of the disease, IgM VCA and IgG VCA may be present; lgG EA and lgG EBNA are necessarily detected. In the atypical course of the chronic form, lgM VCA is absent, there may be lgG VCA, lgG EA and lgG EBNA are present.
Determination of the presence of antibodies is carried out on samples of venous blood and saliva. In the absence of infection, antibodies are not detected. In the acute form of the disease, lgM VCA is found; lgG VCA and lgG EA may be present; lgG EBNA is missing. In the acute phase of the chronic form of the disease, IgM VCA and IgG VCA may be present; lgG EA and lgG EBNA are necessarily detected. In the atypical course of the chronic form, lgM VCA is absent, there may be lgG VCA, lgG EA and lgG EBNA are present.
In cases where the pathogen is in a latent state, lgM VCA and lgG VCA are absent, and lgG EA and lgG EBNA are noted. In the state of recovery after drug treatment, only lgG EBNA is present. In the reactivation phase in the chronic form of the disease, all types of immunoglobulins are found. In the presence of malignancies caused by EBV, a blood test gives the following result: the absence of lgM VCA and a low probability of the presence of lgG EBNA, but a significantly elevated level of lgG VCA and lgG EA.
Deciphering the results
 Positive result, i.e. the presence of infection can be caused by the following reasons: acute form of mononucleosis; active phase of the chronic form of infection; tumor formations; past infection within up to six months after recovery. A false positive result can be obtained if the preparatory period is violated or the sample is taken incorrectly. The result of the analysis can be affected by hemolysis of the sample taken, an increased concentration of lipids, bacterial contamination of the vessel in which the sample is located. A false positive assessment may occur with the following diseases: toxoplasmosis, cytomegalovirus infection, other types of herpes, immunodeficiency.
Positive result, i.e. the presence of infection can be caused by the following reasons: acute form of mononucleosis; active phase of the chronic form of infection; tumor formations; past infection within up to six months after recovery. A false positive result can be obtained if the preparatory period is violated or the sample is taken incorrectly. The result of the analysis can be affected by hemolysis of the sample taken, an increased concentration of lipids, bacterial contamination of the vessel in which the sample is located. A false positive assessment may occur with the following diseases: toxoplasmosis, cytomegalovirus infection, other types of herpes, immunodeficiency.
Negative result, i.e. the absence of all markers can be recorded in the following cases: absence of EBV; incomplete incubation period of infection; the end of the disease (after 6 months after the real end of the disease); latent state of pathogens (a person is only a carrier of the virus). If there is any doubt about the results of the analysis, the study should be repeated after 12-14 days.
Analysis using the PCR method
The use of an analysis for EBV using the ELISA method often cannot give an accurate diagnosis, which requires additional clarifying studies. High diagnostic accuracy is provided by an analysis based on the polymer chain reaction (PCR) method with the detection of viral DNA. A sample of blood, urine, sputum, saliva, amniotic fluid from pregnant women is taken for research.
Most often, studies are carried out on venous blood. The PCR method is an addition to analyzes using ELISA in cases where this analysis does not give an unambiguous interpretation of the results. The use of PCR in blood tests is effective only in acute forms of the disease and exacerbation phases. In chronic forms and to assess the correctness of treatment, this blood test is not used. The use of such studies for newborns is especially recommended. More informative in determining the DNA of the virus in chronic and atypical forms is the analysis of saliva samples.
In addition to blood and saliva samples, Epstein-Barr virus can be detected additionally by sweating, scraping of epithelial cells of the nasal mucosa, scraping of the epithelium of the oropharynx, cerebrospinal fluid, ejaculate, scraping of epithelial cells of the urogenital canal.
Epstein-Barr infection is caused by a virus that belongs to the herpes virus family. The most common manifestation of this infection is mononucleosis. However, Epstein-Barr virus can also cause the development of tumors such as Burkitt's lymphoma and nasopharyngeal cancer.
Epstein-Barr virus. Photo from en.wikipedia.org
Even in the scientific literature, one can find many readings of the name of the disease: Epstein-Barr infection, Epstein-Barr, etc. However, there should be no disagreement here. Sir Michael Epstein, the famous British virologist, is a man. Virologist Yvonne Barr is a woman. Therefore, the disease is called Epstein-Barr infection.
History of discovery and study
Infectious mononucleosis was first described in the late 19th century. Doctors of that time knew this disease as an acute glandular fever, occurring with symptoms of lymphadenopathy (enlargement of the lymph nodes), enlargement of the liver and spleen against the background of an increase in body temperature.
However, many more years passed before the causative agent of infectious mononucleosis was identified. This is largely due to the fact that scientists did not take into account the widest prevalence of the disease, which is why most people are seropositive, i.e. have antibodies to the virus in their blood.
In 1964, Epstein and Barr described a virus that they found in Burkitt's lymphoma cells. This infectious agent was later named Epstein-Barr (EBV).
In 1968, Henle reported a possible link between mononucleosis and the Epstein-Barr virus. This assumption was confirmed in 1971 in a study by Sawyer et al.
Disease prevalence
It is believed that by the age of 25, 90% of the population are carriers of the Epstein-Barr virus. Infection can take the form of acute mononucleosis, but is often completely asymptomatic.
Both women and men suffer from EBV with the same frequency. The likelihood of the disease does not depend on race. Among people with low incomes, the prevalence of EBV carriage is higher, but the disease is more often latent in them.
After the acute phase of the disease, a person remains a carrier, which is typical for the entire family of herpes viruses.
How is EBV transmitted?
The virus is transmitted only from person to person and is contained in the oropharyngeal mucus and saliva of people who first fell ill for 12-18 months. In 20-30% of them, EBV can be detected in saliva throughout life.
The virus is transmitted by airborne droplets with saliva and through household items, but is not very contagious.
Based on the results of epidemiological studies, it is known that the frequency of the appearance of antibodies to EBV in previously uninfected students, whose roommates are carriers of the virus, does not differ from the average numbers in the student environment.
The virus can also enter the body of a previously healthy person during a blood transfusion or bone marrow transplant.
The incubation period of the disease is from 30 to 50 days, but in young children it can be greatly reduced.
Symptoms of infectious mononucleosis
The acute phase of the disease usually lasts 2-3 weeks, but can be delayed for a longer period.
Complaints
Typically, patients with acute infection complain of sore throat and abdominal pain, headaches, muscle pain, fever, difficulty in nasal breathing, and nausea.
Sore throat is the most common symptom of mononucleosis. Gradually increasing during the first week, pain can be very pronounced.
Headache also appears in the first week and may be felt behind the eyes.
Abdominal pain is associated, as a rule, with an enlarged spleen, therefore it is felt in the left upper quadrant of the abdomen. Nasal breathing may be impaired due to enlargement of the nasopharyngeal tonsils (adenoids).
Body temperature rises to 38-39 degrees.
Objective symptoms
Objectively, infectious mononucleosis is manifested by a picture of tonsillopharyngitis (tonsillitis), an increase in lymph nodes throughout the body, an increase in the liver and spleen. A rash may also appear.
When examining the throat, you can see an increase and redness of the palatine tonsils. In about a third of cases, a yellowish thick inflammatory fluid is found in the lacunae of the tonsils. Often, small submucosal hemorrhages are visible on the border of the soft and hard palate. The picture of inflammation in the throat with mononucleosis is similar to the usual lacunar tonsillitis and is often mistaken for it.
When examining the nasopharynx through the nose or through the mouth with a special mirror, the doctor may note an increase and redness of the nasopharyngeal tonsil.
Lymph nodes with mononucleosis increase symmetrically. The posterior cervical, anterior cervical, submandibular, axillary, inguinal, ulnar groups of lymph nodes are affected. On palpation (palpation), they are slightly painful and mobile.
Enlargement of the liver and spleen is common. At the same time, jaundice in patients with mononucleosis is relatively rare.
The spleen rapidly increases in the first week of illness. This carries the risk of organ rupture with minimal trauma. Cases of spontaneous rupture of the spleen have been described.
On the skin throughout the body in a small number of cases (up to 15%), a pale maculopapular rash may occur. The likelihood of a rash increases significantly if mononucleosis is mistakenly started to be treated with penicillin antibiotics. This treatment is relatively common when a mononuclear throat infection is mistaken for a common strep throat.
Diagnostics
Diagnosis of infectious mononucleosis is based on the clinical picture and laboratory tests.
The three classic laboratory symptoms of mononucleosis are:
- lymphocytosis (an increase in the number of lymphocytes in the blood test - blood cells responsible for fighting viruses);
- the presence in the blood test of at least 10% of mononuclear cells - atypical lymphocytes;
- positive serological tests (detection of antibodies to EBV in the blood).
General blood analysis
In a general blood test, you can usually see leukocytosis - an increase in the number of white blood cells in the blood. This is a non-specific sign of the presence of an infection in the body, along with an increase in ESR.
Lymphocytosis is observed in 80-90% of people with mononucleosis. Usually, with EBV infection, up to 20-40% of atypical mononuclear cells can be detected in the blood. But sometimes these cells can be less than 10%. Their absence does not exclude the diagnosis of mononucleosis.
Liver tests
Almost all patients with mononucleosis have a temporary increase in the level of bilirubin and liver enzymes - aminotransferases. Changes in the biochemical characteristics of liver function can be observed up to 3 months. However, this is not a specific sign of the disease.
Serological method
In practice, most often, a clinical picture and a general blood test are sufficient to make an accurate diagnosis. In some cases, it may be necessary to determine antibodies to EBV.
Already in the incubation period of mononucleosis in the blood serum, IgM antibodies of the acute phase to the Epstein-Barr virus can be detected. A few months after the disappearance of the symptoms of the disease, IgM is no longer detected in the blood.
A person who has had an Epstein-Barr virus infection retains IgG antibodies for life .
PCR for EBV infection
 PCR (polymerase chain reaction) is of limited value in mononucleosis. The method can determine the presence of the genetic material of the virus in the blood serum. In the case of asymptomatic carriage of the Epstein-Barr virus, the detection of viral DNA in the blood often indicates a reactivation of the infectious process. Also, PCR can act as a means of monitoring the effectiveness of treatment in complicated cases.
PCR (polymerase chain reaction) is of limited value in mononucleosis. The method can determine the presence of the genetic material of the virus in the blood serum. In the case of asymptomatic carriage of the Epstein-Barr virus, the detection of viral DNA in the blood often indicates a reactivation of the infectious process. Also, PCR can act as a means of monitoring the effectiveness of treatment in complicated cases.
How to Treat an Epstein-Barr Virus Infection
With the Epstein-Barr virus, the human immune system usually copes on its own and no specific treatment is needed. All that is needed is to provide the body with optimal conditions for recovery (rest, adequate fluid intake).
Medical treatment for mononucleosis is aimed at relieving symptoms. The patient is given painkillers, antipyretic drugs.
In rare cases, when the enlargement of the tonsils is so pronounced that it causes a narrowing of the airway, steroid hormones are prescribed for anti-inflammatory and decongestant purposes.
Diet changes are not required for mononucleosis unless the person is unable to swallow due to a sore throat and enlarged palatine tonsils.
There is no need to isolate the patient for the duration of treatment due to the low contagiousness of the infection.
A patient suffering from mononucleosis can be treated on an outpatient basis (without hospitalization). In rare cases (rupture of the spleen), surgical treatment is necessary.
It is because of the risk of rupture of the spleen during the treatment of mononucleosis that restrictions are placed on the patient's physical activity. Heavy lifting and contact sports should be avoided for 2-3 weeks. Some doctors consider justified and longer periods - up to 2 months after recovery.
Prognosis, complications, risk of chronic form
The prognosis for infectious mononucleosis in people without immunodeficiency is favorable. Sometimes patients (more often women) experience chronic fatigue for up to 2 years after treatment.
Complications of EBV infection include narrowing of the airways, rupture of the spleen, meningitis, hepatitis, thrombocytopenia (a decrease in the number of blood cells responsible for stopping bleeding), and hemolytic anemia (anemia). However, they are rare.
More often there are complications such as otitis media and sinusitis.
In addition to infectious mononucleosis, the virus can cause the development of certain types of lymphoma, as well as carcinoma of the nasopharynx. However, given the almost universal prevalence of EBV in the population, this risk is low. The specific mechanisms that determine tumor development in only some carriers of the virus are not clear.